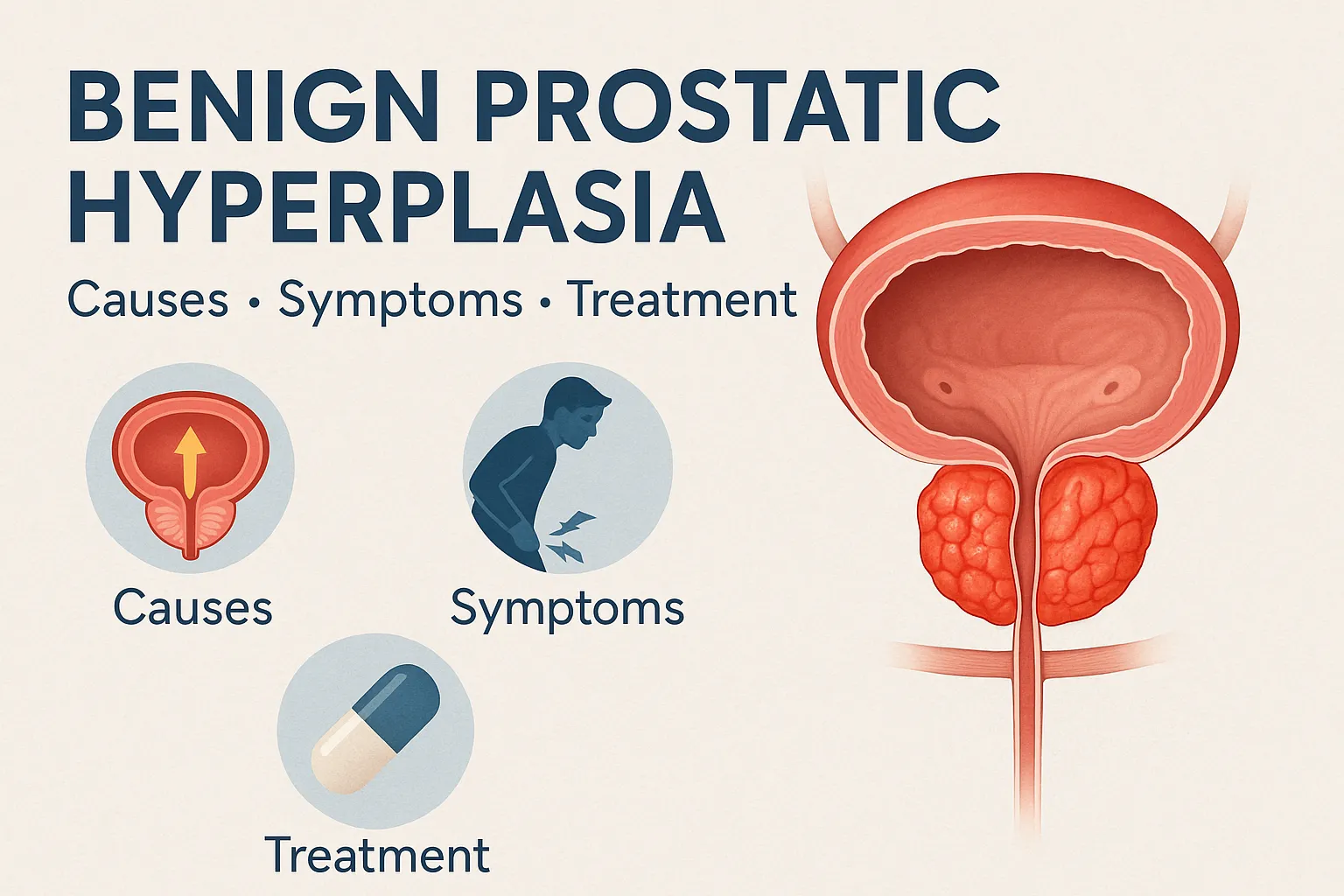
Benign Prostatic Hyperplasia (BPH) is one of the most common health conditions that affects men as they grow older. It occurs when the prostate gland — a small, walnut-shaped organ located below the bladder — enlarges and begins to interfere with normal urine flow.
While BPH is not cancerous and does not increase the risk of prostate cancer, it can significantly impact quality of life. Many men with BPH experience frustrating urinary symptoms such as frequent trips to the bathroom at night, difficulty starting urination, or the sensation of an incompletely emptied bladder.
The good news is that BPH is manageable. With timely diagnosis and treatment, men can reduce discomfort and avoid long-term complications.
What is Benign Prostatic Hyperplasia?
BPH is a non-cancerous enlargement of the prostate gland. The prostate plays an important role in male reproductive health by producing seminal fluid, which nourishes and transports sperm.
As men age, the prostate naturally grows. In some cases, this growth becomes excessive, compressing the urethra (the tube that carries urine from the bladder out of the body). This narrowing leads to difficulty in urination and other lower urinary tract symptoms (LUTS).
It is estimated that about 50% of men aged 50 and above show some signs of BPH, and the prevalence rises to nearly 90% in men over 80.
Causes & Risk Factors
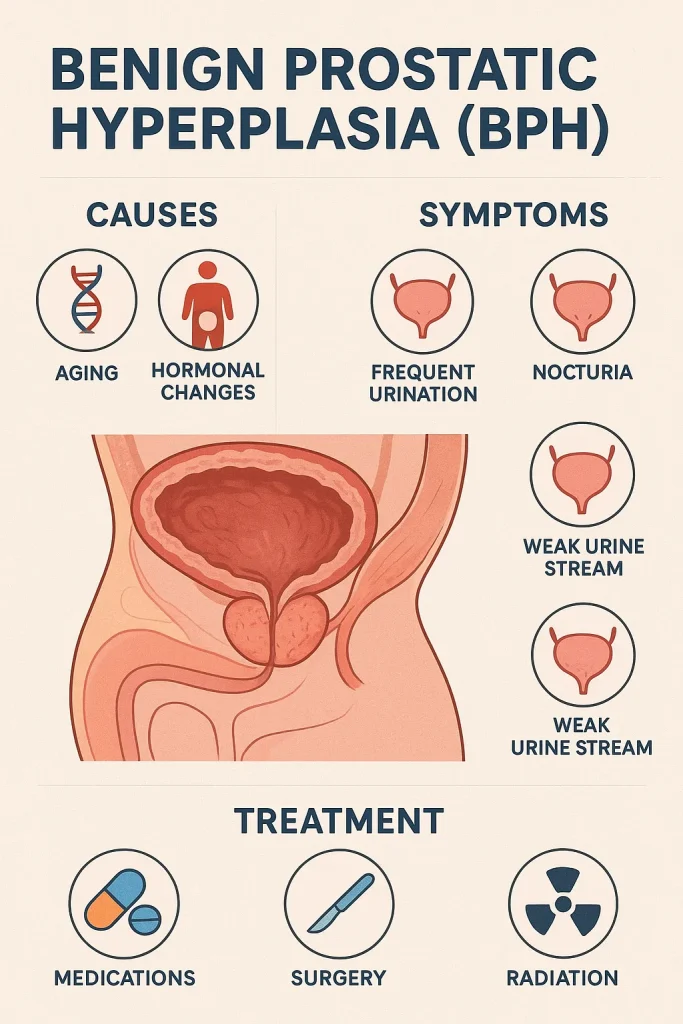
The exact cause of BPH isn’t fully understood, but several factors contribute to its development:
1.1 Natural Aging Process
BPH is closely linked with age. As men get older, cell growth within the prostate accelerates, increasing its size.
1.2 Hormonal Changes
Hormones play a central role. Testosterone, the male sex hormone, is converted into dihydrotestosterone (DHT) within the prostate. High levels of DHT are believed to stimulate prostate cell growth. A relative decline in testosterone with age, paired with steady estrogen levels, may also contribute.
1.3 Family History
Men with close relatives (father, brother) diagnosed with BPH are more likely to develop the condition themselves.
1.4 Lifestyle Factors
- Obesity increases the risk due to hormonal imbalances.
- Lack of exercise reduces overall metabolic health, worsening symptoms.
- Alcohol and caffeine can irritate the bladder, making urinary symptoms more noticeable.
Symptoms of BPH
BPH symptoms vary in severity, but they usually fall under two categories: obstructive (due to blockage of urine flow) and irritative (related to bladder overactivity).
Common symptoms include:
- Urinary frequency: The need to urinate often, especially during the night (nocturia).
- Weak or interrupted urine stream: A reduced flow, often stopping and starting.
- Difficulty starting urination: Hesitancy before urine begins to flow.
- Incomplete bladder emptying: A lingering feeling that the bladder isn’t fully emptied.
- Urgency and dribbling: Sudden strong urges to urinate, sometimes followed by leakage.
These symptoms can interfere with sleep, daily activities, and overall well-being.
Complications if Left Untreated
While BPH itself is not life-threatening, untreated cases can lead to serious complications:
- Urinary Tract Infections (UTIs): Poor bladder emptying allows bacteria to thrive.
- Bladder stones: Stagnant urine can crystallize, leading to painful stones.
- Kidney damage: Prolonged pressure from urinary retention can harm kidney function.
- Acute urinary retention: A sudden inability to urinate, which is a medical emergency requiring immediate catheterization.
Diagnosis of BPH
Proper diagnosis ensures BPH is distinguished from more serious conditions like prostate cancer. Evaluation typically includes:
- Patient history & symptom check: Using tools like the International Prostate Symptom Score (IPSS).
- Digital Rectal Exam (DRE): A doctor physically checks prostate size and texture.
- Urine & blood tests: To rule out infections and measure Prostate-Specific Antigen (PSA) levels, which help exclude prostate cancer.
- Ultrasound or imaging: In cases where more detail is needed, to assess the bladder, kidneys, and prostate size.
Treatment Options
Treatment depends on the severity of symptoms, overall health, and patient preference.
Lifestyle & Home Remedies
- Reduce caffeine and alcohol: Both irritate the bladder and worsen urgency.
- Bladder training: Scheduled bathroom visits help improve bladder control.
- Fluid management: Limiting fluids before bedtime reduces nocturia.
- Exercise & weight management: Improves overall urinary and metabolic health.
Medications
- Alpha-blockers
- Examples: Tamsulosin, Alfuzosin, Doxazosin.
- Function: Relax muscles of the prostate and bladder neck, easing urine flow.
- Onset: Rapid relief, often within days.
- 5-Alpha Reductase Inhibitors
- Examples: Finasteride, Dutasteride.
- Function: Block conversion of testosterone to DHT, reducing prostate size over months.
- Best suited for men with significantly enlarged prostates.
- Combination Therapy
- Alpha-blocker + 5-ARI provides faster relief and long-term size reduction.
- Role of Tadalafil (Cialis)
- Originally developed for erectile dysfunction (ED), Tadalafil also relaxes bladder and prostate muscles.
- Approved for men with both BPH and ED, improving urinary symptoms and sexual function simultaneously.
Minimally Invasive Procedures
For men not responding to medication:
- Transurethral Microwave Therapy (TUMT): Heat destroys excess prostate tissue.
- UroLift System: Small implants hold the enlarged prostate tissue away from the urethra.
Surgery (for severe cases)
- TURP (Transurethral Resection of the Prostate): The gold standard; removes part of the prostate.
- Laser surgery: Uses laser energy to vaporize or enucleate prostate tissue.
- Prostatectomy: Entire removal of the prostate, usually for very large glands.
Living With BPH
Managing BPH is often a long-term process. With the right care, men can live comfortably:
- Daily adjustments: Limiting late-night fluid intake, avoiding bladder irritants, and practicing pelvic floor exercises.
- Regular check-ups: To monitor progression and adjust treatment if needed.
- Mental health: Anxiety and embarrassment about urinary symptoms are common; discussing openly with doctors and partners is important.
FAQs
Is BPH the same as prostate cancer?
No. BPH is benign (non-cancerous). However, both conditions may cause similar urinary symptoms, so medical evaluation is essential.
At what age does BPH usually start?
It typically begins after age 40 and becomes increasingly common with each decade.
Can diet and exercise help?
Yes. A balanced diet rich in fruits, vegetables, and omega-3 fatty acids, along with regular exercise, can reduce symptoms and improve overall health.
Will I need surgery for BPH?
Not always. Many men manage well with lifestyle changes or medication. Surgery is reserved for severe cases or when complications develop.
Conclusion
Benign Prostatic Hyperplasia (BPH) is a common and manageable condition in older men. While it is not cancer, it can significantly impact daily life through urinary problems.
Fortunately, a wide range of treatments — from lifestyle adjustments to advanced surgical procedures — are available. Early diagnosis is key to preventing complications and improving quality of life.
If you experience persistent urinary symptoms, don’t ignore them. Speak to your doctor, explore your treatment options, and take proactive steps to protect your urinary and overall health.


Comments (0)
Leave A Comment